Causes and Prevention of Premature Ovulation During IVF
During in vitro fertilization (IVF), timing is everything. One of the most delicate parts of the process is controlling when ovulation occurs so that eggs can be retrieved before they are released. However, sometimes the body doesn’t follow the plan, and premature ovulation happens.
If you’ve asked yourself, “What causes premature ovulation during IVF?” you’re not alone. Premature ovulation can disrupt an IVF cycle because it leads to the release of mature eggs before they can be collected, leaving fewer or even no eggs available for fertilization.
This article explains what premature ovulation is, what causes it, how it affects your IVF outcome, and the strategies fertility specialists use to prevent it.
What Is Premature Ovulation in IVF?
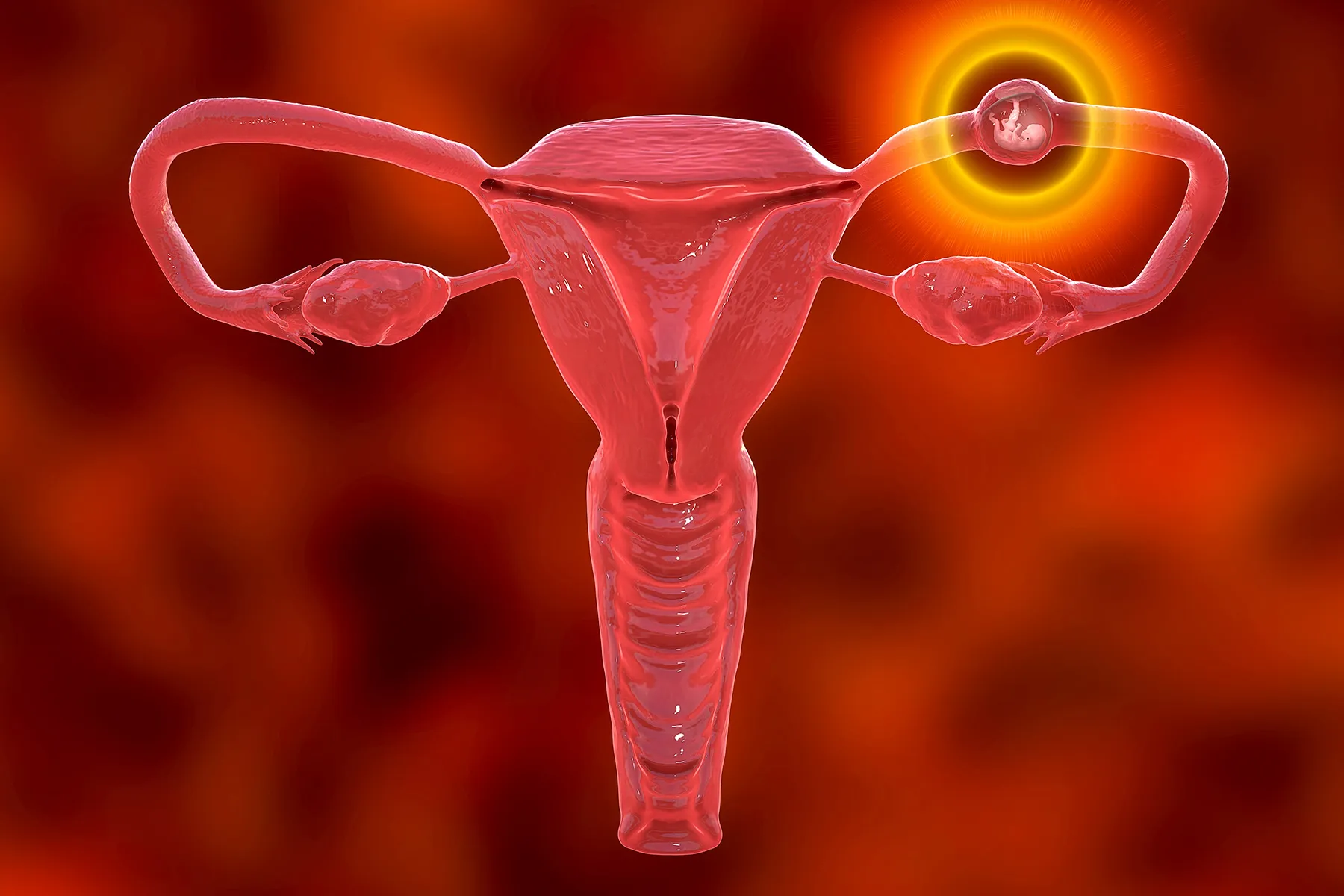
Under normal conditions, ovulation happens when a mature egg is released from the ovarian follicle around the middle of a woman’s menstrual cycle. During IVF, however, the process is medically controlled with hormonal medications to stimulate multiple follicles and prevent them from releasing their eggs too soon.
Premature ovulation occurs when one or more follicles rupture and release their eggs before the scheduled egg retrieval. This can happen despite the use of fertility medications designed to suppress natural ovulation.
When this occurs, the eggs that were supposed to be retrieved are lost into the abdominal cavity, where they can no longer be used for IVF.
Why Premature Ovulation Matters
Premature ovulation can have a major impact on the IVF cycle:
- Fewer eggs retrieved: If eggs are released before retrieval, the embryologist has fewer or no eggs to fertilize.
- Cycle cancellation: In severe cases, an IVF cycle may need to be stopped and restarted later.
- Emotional and financial strain: A canceled cycle can be disheartening and expensive, especially after days of hormone injections and monitoring.
Fortunately, premature ovulation is relatively rare thanks to modern IVF protocols, and there are effective ways to prevent it.
What Causes Premature Ovulation During IVF
Premature ovulation can result from a combination of hormonal, biological, and medication-related factors. Below are the most common causes:
1. Natural Hormonal Surge
The most frequent cause is a premature luteinizing hormone (LH) surge. LH is responsible for triggering ovulation in a natural cycle. In IVF, if the LH level rises before the doctor administers the trigger shot (usually hCG or Lupron), ovulation can occur earlier than expected.
This is why IVF patients undergo frequent blood tests and ultrasounds — to detect any early signs of a hormone surge and adjust medications as needed.
2. Inadequate Suppression of Ovulation
IVF protocols use medications like GnRH agonists or antagonists to suppress natural ovulation. However, if the dosage isn’t sufficient or the timing isn’t precise, the suppression may fail, allowing follicles to release eggs prematurely.
Factors that can affect medication response include:
- Individual differences in hormone sensitivity
- Missed or delayed medication doses
- Rapid ovarian response to stimulation drugs
Your doctor carefully adjusts medication schedules to minimize this risk.
3. Advanced Ovarian Response
Some patients, particularly younger women or those with polycystic ovary syndrome (PCOS), may have an overactive ovarian response to stimulation. Their follicles grow and mature quickly, which can increase the likelihood of early ovulation if not closely monitored.
This is why fertility specialists perform frequent ultrasounds and hormone tests to track follicle size and hormone levels daily near the end of stimulation.
4. Missed or Late Trigger Shot
The trigger shot, usually administered 36 hours before egg retrieval, plays a key role in timing ovulation. If it’s taken too late or incorrectly, ovulation may happen naturally before retrieval can occur.
For this reason, IVF clinics provide precise instructions and timing for administering the trigger shot, often down to the minute. Following these instructions carefully helps prevent premature egg release.
5. Individual Biological Variability
Every woman’s hormonal system is slightly different. Even with perfect adherence to the medication protocol, some women’s bodies may respond faster or differently to stimulation. This variability means that occasional premature ovulation can occur despite close medical management.
In such cases, the fertility team may adjust the next cycle’s medications or consider a different suppression protocol.
Does Premature Ovulation Affect Egg Quality?
In most cases, premature ovulation affects egg availability more than egg quality, but timing still plays an important role in fertility outcomes.
When ovulation occurs too early, eggs are often released before they’ve completed final maturation. Immature or partially mature eggs are less likely to fertilize successfully or develop into healthy embryos. Even if some eggs remain in the ovaries for retrieval, their maturity and developmental potential might be lower.
Furthermore, if eggs are lost into the fallopian tubes or abdominal cavity, they can’t be retrieved at all, reducing the overall egg count for that IVF cycle.
However, premature ovulation does not cause long-term damage to the ovaries or future cycles. Once the cause is identified, whether hormonal or medication-related, your doctor can modify the protocol for better synchronization in the next cycle, improving both egg quantity and quality outcomes.
How to Prevent Premature Ovulation During IVF
The good news is that premature ovulation is preventable in most cases. Clinics use several strategies to minimize the risk:
1. Hormone Suppression Medications
Medications such as GnRH antagonists (like Cetrotide or Ganirelix) are used to block the body’s natural LH surge. These are typically started midway through ovarian stimulation once follicles begin to mature.
For patients with unpredictable hormonal responses, GnRH agonist protocols may be used instead to maintain tighter control.
2. Frequent Monitoring
Frequent blood tests and ultrasounds allow fertility specialists to track hormone levels and follicle development closely. If an early LH rise is detected, adjustments can be made immediately, either triggering ovulation early or increasing suppression medication.
3. Strict Timing for Trigger Shots
Since timing is critical, patients are instructed to take their trigger shot exactly 36 hours before retrieval. Even a few hours’ difference can alter results. Clinics often provide a written schedule and direct communication to ensure accuracy.
4. Customized Stimulation Protocols
Your fertility doctor may tailor your medication plan based on your previous IVF response, age, and ovarian reserve. For example, women prone to early ovulation may start antagonist medications earlier or use dual triggers (a combination of hCG and Lupron) for tighter control.
Personalized protocols greatly reduce the risk of premature ovulation.
Signs of Premature Ovulation
It’s not always easy to detect premature ovulation without medical monitoring, but some subtle signs can appear:
- Sudden pelvic discomfort or cramping before retrieval
- Drop in estrogen levels (E2) detected through blood tests
- Presence of free fluid on ultrasound (indicating follicle rupture)
If these signs appear, your doctor may proceed with an early retrieval or, in some cases, cancel the cycle.
Can Premature Ovulation Be Fixed?
If premature ovulation is detected early enough, sometimes a rescue retrieval can be performed. This means the procedure is done a few hours earlier than planned to collect any remaining eggs.
If all eggs have already been released, the cycle may need to be postponed, and your doctor will adjust medications in the next round to better control hormone levels.
Although frustrating, this does not mean IVF will fail in the future. With the right protocol adjustments, many patients go on to have successful cycles afterward.
Final Thoughts
If you’ve experienced or worry about premature ovulation during IVF, remember that it’s not your fault; it’s a biological response that can happen even under expert supervision.
The key is close monitoring, proper medication timing, and a personalized treatment plan. With these measures, fertility specialists can dramatically reduce the risk of premature ovulation and keep your IVF journey on track.
At The Bridge Clinic, our fertility specialists use advanced IVF protocols and continuous monitoring to optimize every step of your treatment, including ovulation control and egg retrieval timing.
Reach out to The Bridge Clinic today to schedule a consultation and learn how we can help you achieve the best possible outcome on your IVF journey.
Follow us on our social media channels below:
Explore our related articles below:








